End of Life and Palliative Care
Clinical Vignette: You are an IMT doctor working on the acute medical unit.
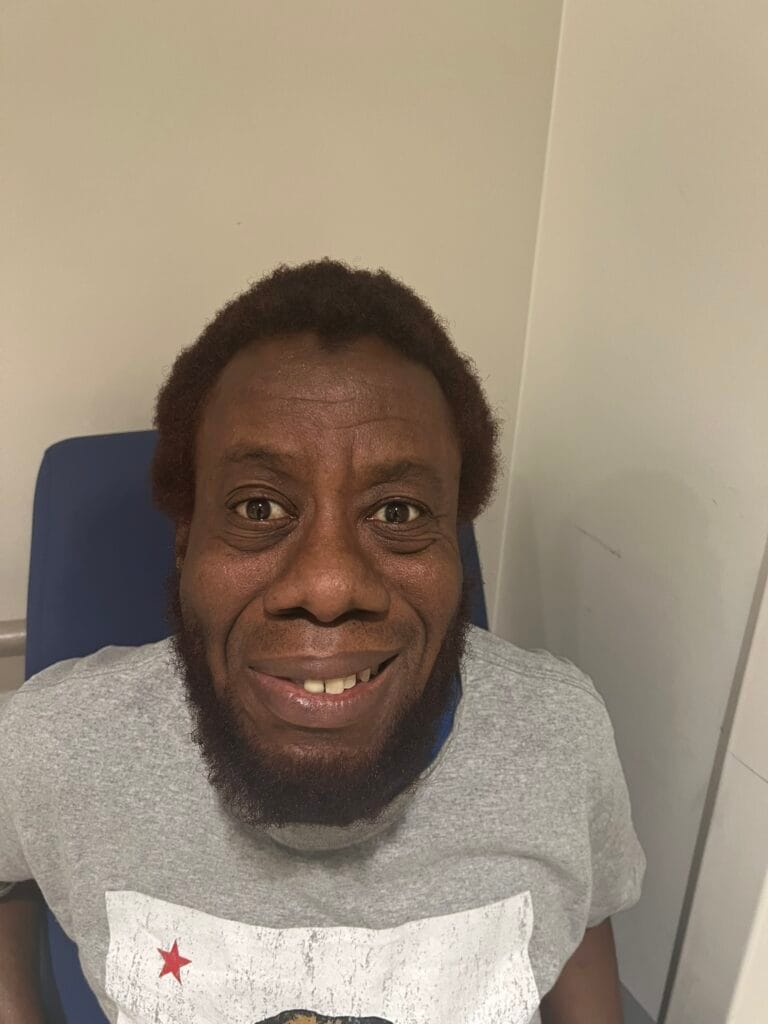
You are asked to speak to Mr David Thompson, a 74-year-old man with metastatic colorectal cancer, admitted with sepsis and worsening functional decline.
Despite appropriate treatment, he has continued to deteriorate. The medical team feels that he is approaching the end of his life, and a decision has been made that the focus of care should be palliative
What This Station Is Testing?
- Rapport and empathy
- Clear, compassionate communication
- Explaining end-of-life care without removing hope
- Exploring patient values and wishes
- Shared decision-making
- Planning and safety netting
Model Consultation Structure
Introduce and set expectations
Explore understanding of illness and prognosis
Ask permission to discuss end-of-life care
Explain palliative focus clearly
Explore patient values, fears, and priorities
Agree a plan aligned with patient wishes
Summarise, safety net, and close
Opening Framework
Aim: Create a safe environment, set the agenda, check understanding, and obtain permission.
Key steps:
Introduce yourself and your role
Acknowledge the seriousness of the situation
Check the patient’s understanding so far
Ask permission to discuss future care
Model opening:
“Hello, my name is Dr ___, one of the medical doctors looking after you today. Before we start, can I check that you’re comfortable and that this feels like a good time to talk?”
“I wanted to talk to you about how things are going with your illness and to discuss how we can best support you moving forward. Would that be okay?”
Empathy (use early):
“I can see this has been a very difficult time for you.”
Core Content - SPIKES Framework
S – Setting and Listening Skills
Sit at eye level
Use open body language
Speak calmly and clearly
Allow pauses and silence
Model phrasing:
“I want to make sure we have time and privacy for this conversation.”
P – Patient’s Perception
Establish what the patient understands about their condition and prognosis.
Model phrasing:
“Before we go any further, can I ask what you understand about how things are going with your illness at the moment?”
Listen carefully and correct misunderstandings gently.
I – Invitation
Seek permission to discuss end-of-life and palliative care.
Model phrasing:
“Would it be okay if we talked about what’s most important to you now, and how we can focus your care on comfort and quality of life?”
“Some people like to have family involved in these discussions would you want anyone else here with you?”
K – Knowledge (Explaining End-of-Life & Palliative Care)
Explain clearly, without jargon or abruptness.
Key principles:
Palliative care ≠ giving up
Focus on comfort, dignity, and symptom control
Be honest but compassionate
Model explanation:
“Although we’re still treating problems as they arise, the illness has reached a stage where treatments aimed at cure are no longer helping.”
“At this point, the kindest and most appropriate approach is to focus on keeping you comfortable, managing symptoms, and supporting you and your family.”
Avoid terms like nothing more we can do.
E – Explore Emotions and Values
Pause and explore emotional response.
Model phrasing:
“I know this may be very hard to hear. How does this feel for you?”
Explore values:
Comfort vs longevity
Being at home vs hospital
Fear of pain or distress
Important events or wishes
Respond empathetically and validate feelings.
S – Strategy and Summary
Agree a clear, patient-centred plan.
Key elements:
Symptom control (pain, breathlessness, anxiety)
Ceilings of care (ward-based, no escalation)
DNACPR if appropriate
Place of care and preferred place of death
Model phrasing:
“Based on what you’ve told me, I think focusing on comfort and quality of life fits best with what matters to you.”
“Does this plan feel right to you?”
Immediate Next Steps
Refer to palliative care team
Optimise symptom control
Document ceilings of care and escalation plans
Offer to involve family and next of kin
Consider community or hospice input
Offer support explicitly:
“Would you like me to contact a family member for you?”
“We can involve the specialist palliative care team today.”
“We can talk about whether being at home or in a hospice would be important to you.”
Key Phrases That Score Marks
“This is about focusing on what matters most to you.”
“Palliative care is about comfort and support, not giving up.”
“We’ll continue to care for you and manage symptoms actively.”
“What’s most important to you right now?”
“What are your biggest worries at the moment?”
“We can review this plan at any time.”
Common Station Pitfalls
Saying “there’s nothing more we can do”
Being vague or overly euphemistic
Avoiding prognosis entirely when appropriate
Not exploring patient priorities
Failing to involve palliative care services
Not summarising the plan clearly
Safetynetting & Close
Invite questions:
“What questions or worries do you have at the moment?”
Summary:
“Today we discussed that your illness has reached a stage where focusing on comfort and quality of life is most appropriate. We’ve talked about managing symptoms, involving the palliative care team and making sure you’re supported.”
Safety net:
“If your symptoms worsen or you feel distressed, please let the nursing staff know immediately we will ensure a care plan is in place in anticipation to any deteriorating symptoms you may be experiencing. These plans will be reviewed regularly to ensure your comfort.”
Offer:
Palliative care nurse presence
Family contact
Written information
Take-Away Box
End-of-life discussions are about honesty, compassion and aligning care with what matters most to the patient.