DNACPR and Ceiling of Care
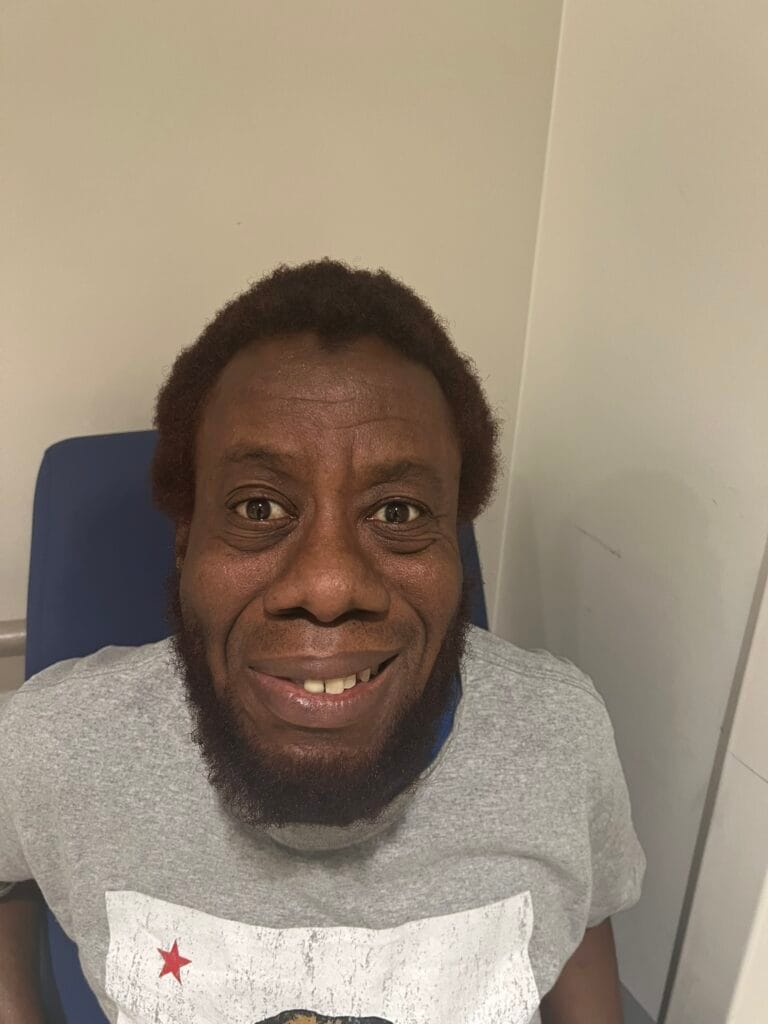
Clinical Vignette: You are an IMT doctor working on the acute medical unit.
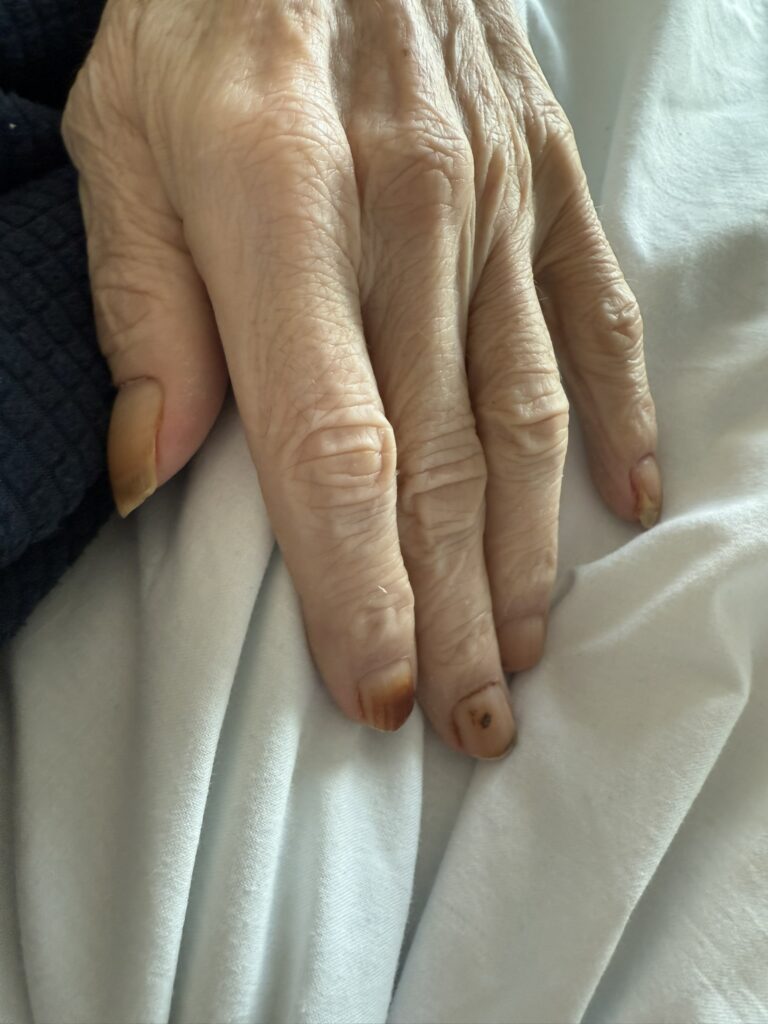
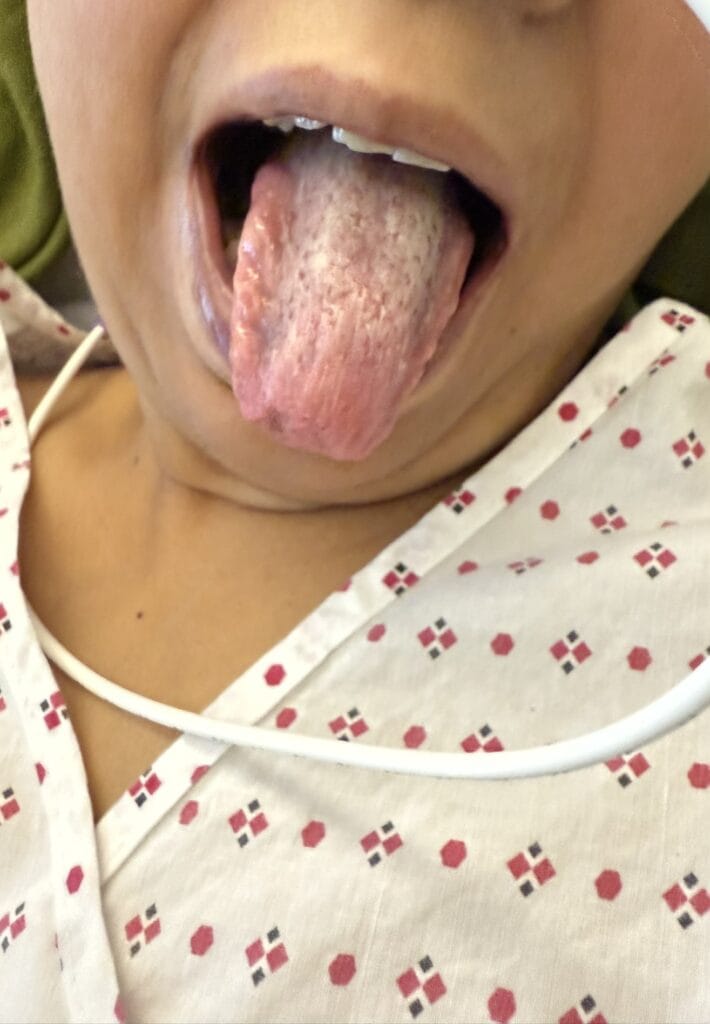
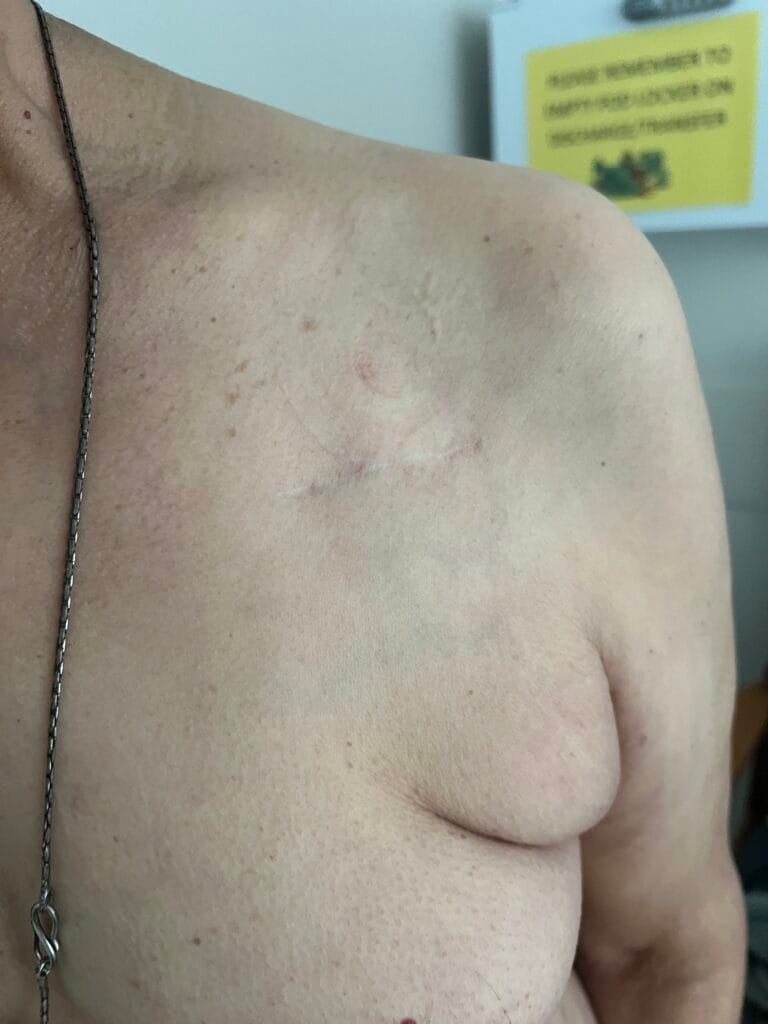
You are asked to speak to Mrs Margaret Lewis, a 82-year-old woman admitted with severe community-acquired pneumonia on a background of advanced heart failure and frailty.
She has deteriorated overnight despite treatment. The consultant has asked you to discuss treatment escalation and DNACPR with her.
What This Station Is Testing?
- Explain the patient’s current condition
- Discuss ceilings of care and DNACPR sensitively
- Explore the patient’s values and wishes
- Address concerns and emotions
- Agree a clear plan and provide reassurance
Model Consultation Structure
- Introduce and set expectations (role, agenda, confidentiality)
- Explore understanding of current illness
- Ask permission to discuss future care
- Explain DNACPR clearly and calmly
- Explore values and concerns
- Agree a plan aligned with the patient’s wishes
- Summarise, safety net, and close
Opening Framework
Aim: Create a safe environment, set the agenda, check understanding, and obtain permission.
Key steps:
Introduce yourself and your role
Acknowledge the seriousness of the situation
Check understanding of current illness
Ask permission to discuss future care
Model opening:
“Hello, my name is Dr ___, one of the medical doctors looking after you today. Before we start, can I check that you’re comfortable and that this feels like a good time to talk?”
“I wanted to talk to you about how you’re doing at the moment and to discuss planning your care going forward. Would that be okay?”
Empathy (use early):
“I can see this has been a difficult admission we can take this at your own pace.”
Core Content - SPIKES Framework
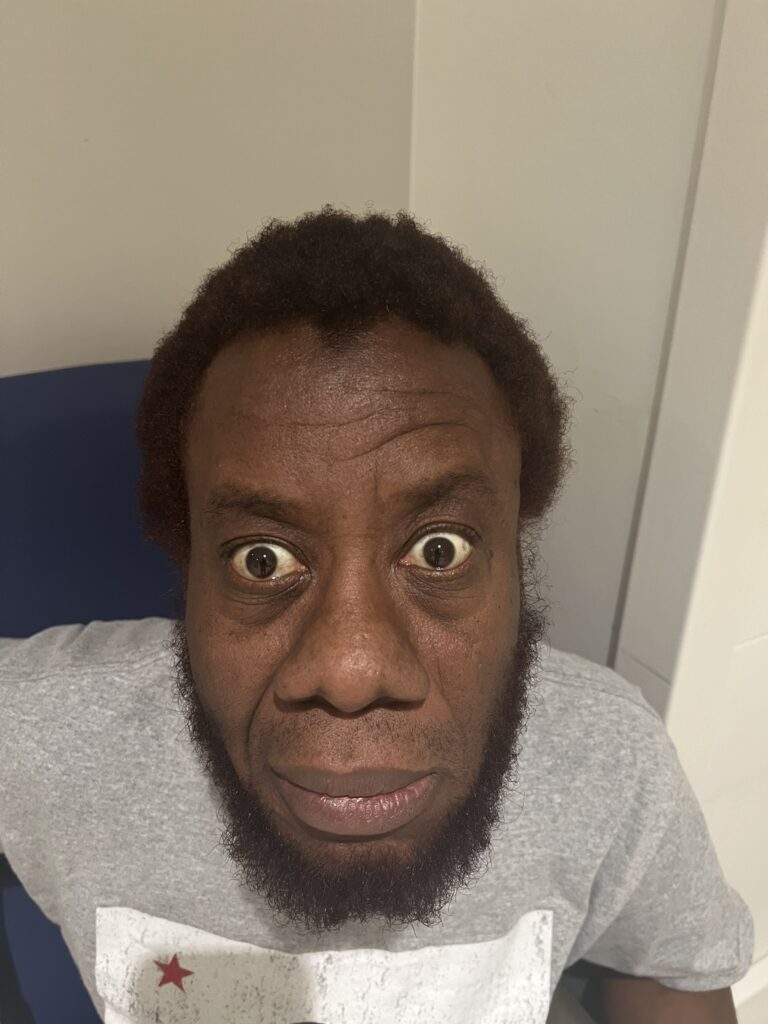
S – Setting and Listening Skills
Sit at eye level
Use open body language
Speak calmly and slowly
Allow pauses
Model phrasing:
“I want to make sure we have time and privacy for this conversation.”
P – Patient’s Perception
Establish what the patient understands.
Model phrasing:
“Before we go any further, can I ask what you understand about how unwell you’ve been?”
Listen carefully and clarify gently.
I – Invitation
Seek permission to discuss escalation and DNACPR.
Model phrasing:
“Would it be okay if we talked about planning your care, including what would be best for you if you became more unwell?”
“Some people like to involve family in these discussions — would you want anyone else here?”
K – Knowledge (Explaining DNACPR)
Explain DNACPR clearly and non-alarmingly.
Key principles:
DNACPR ≠ stopping treatment
Focus on benefit vs burden
Use plain language
Model explanation:
“When someone becomes very unwell, doctors sometimes have to decide whether trying to restart the heart would help or cause more harm. In people with significant medical problems, chest compressions often don’t work and can be traumatic.”
“A DNACPR form means we would continue all appropriate treatments, but we would not attempt chest compressions if your heart were to stop, because it would be unlikely to help you.”
Avoid jargon such as futility or resuscitation algorithms.
E – Explore Emotions and Values
Pause and explore the patient’s priorities.
Model phrasing:
“How does hearing that make you feel?”
“What matters most to you if your health were to get worse?”
Explore:
Independence
Comfort
Fear of suffering
Being at home vs hospital
Respond empathetically and validate concerns.
S – Strategy and Summary
Agree a clear, patient-centred plan.
Key elements:
DNACPR decision (if appropriate)
Ceiling of care (ward-based care, oxygen, IV antibiotics)
What will still be done
Model phrasing:
“Based on what you’ve told me, I think the kindest and most appropriate plan would be to focus on comfort and treatments that help you feel better, without attempting chest compressions.”
“Does that sound in keeping with your wishes?”
Immediate Next Steps
Document DNACPR and escalation plan
Inform the consultant, nursing team and GP
Offer to involve family or next of kin
Consider palliative care or specialist support
Ensure symptom control (breathlessness, pain, anxiety)
Key Phrases That Score Marks
- “This is about making sure your care is right for you.”
- “A DNACPR decision does not mean we stop treating you.”
- “We would continue to treat you actively and keep you comfortable.”
- “What matters most to you?”
- “Does this plan feel right to you?”
- “We can review this decision at any time.”
Common Station Pitfalls
Presenting DNACPR as a tick-box exercise
Sounding like treatment is being withdrawn
Not exploring patient values and wishes
Rushing the conversation
Failing to check capacity
Not summarising clearly
Safetynetting & Close
Invite questions:
“Do you have any questions do you have about what we’ve discussed?”
Summary:
“Today we discussed how unwell you’ve been, what CPR involves, and why it may not be helpful in your situation. We agreed a plan focused on comfort and appropriate treatment, in line with your wishes.”
Safety net:
“If you change your mind or have concerns, please tell us these decisions can always be reviewed.”
Offer:
Nurse presence
Family contact
Written information
Revisit the decision in the future
Take-Away Box
DNACPR discussions are about aligning care with patient values not withdrawing care.