Respiratory Station
Interstitial Lung Disease
Important Physical Signs
General:
- Age (young – CF, TIS // old – COPD, ILD, Lung Malignancy more likely)
- Cachectic (ILD, COPD, Lung Malignancy, CF, Bronchiectasis)
- Tachypnoeic (count respiratory rate on air / oxygen)
- Cushingoid (steroid use)
- Asymmetric chest movement
Cough (productive vs dry)
Peripheral: (hands – arms – face – neck – torso)
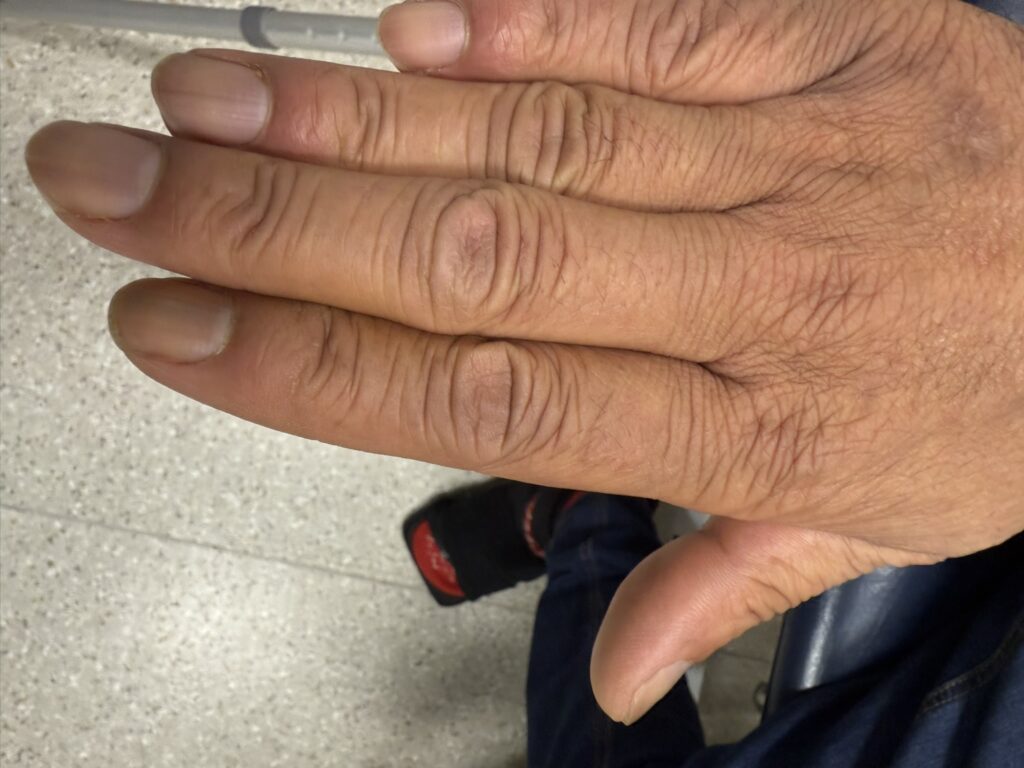
- Hands
- Peripheral cyanosis (blue finger pulp discolouration)
- Tar-stained fingers (check between index and middle fingers smokers)
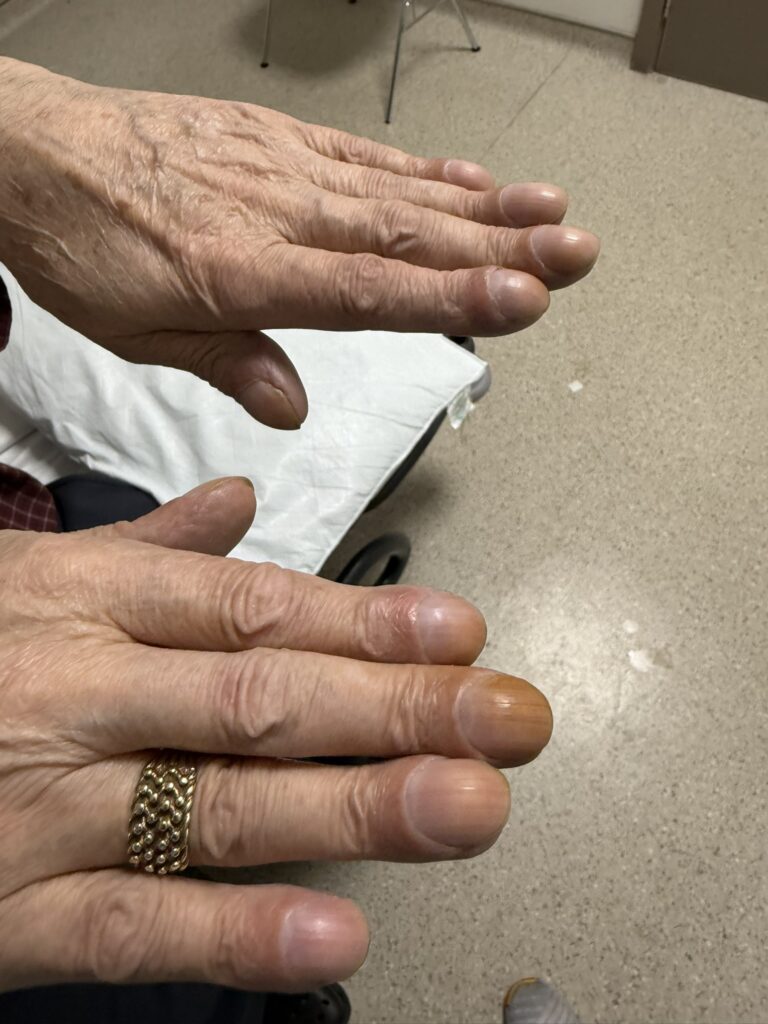
- Rheumatoid hands (RA)
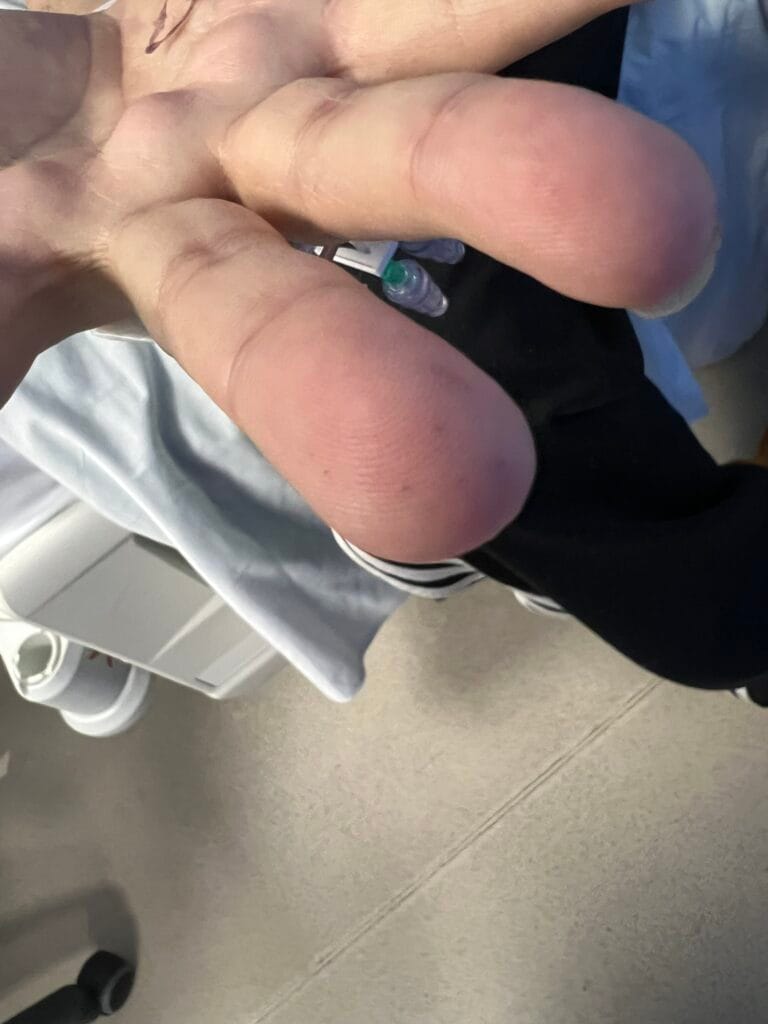
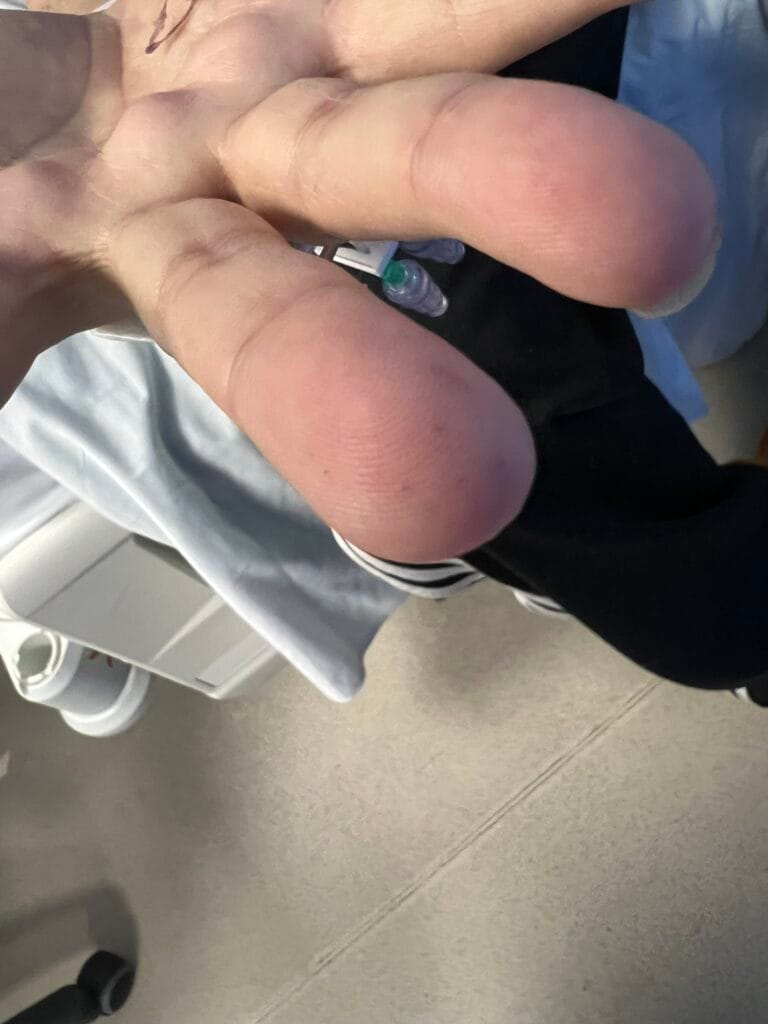
- Clubbing
(suppurative lung disease, idiopathic pulmonary fibrosis) - Sclerodactyly, calcinosis, pulp atrophy, terminal phalanx tufting , Raynaud’s (systemic sclerosis)
- Asterixis (CO2 retention)
- Small muscle wasting (Pancoast tumour)
- Radial pulse (bounding pulse CO2 retention) and respiratory rate (breathless)
- Arms
- Muscle wasting (cachexia in lung malignancy, COPD)
- Bruising (steroid purpura)
- Rheumatoid nodules (elbows, ankles)
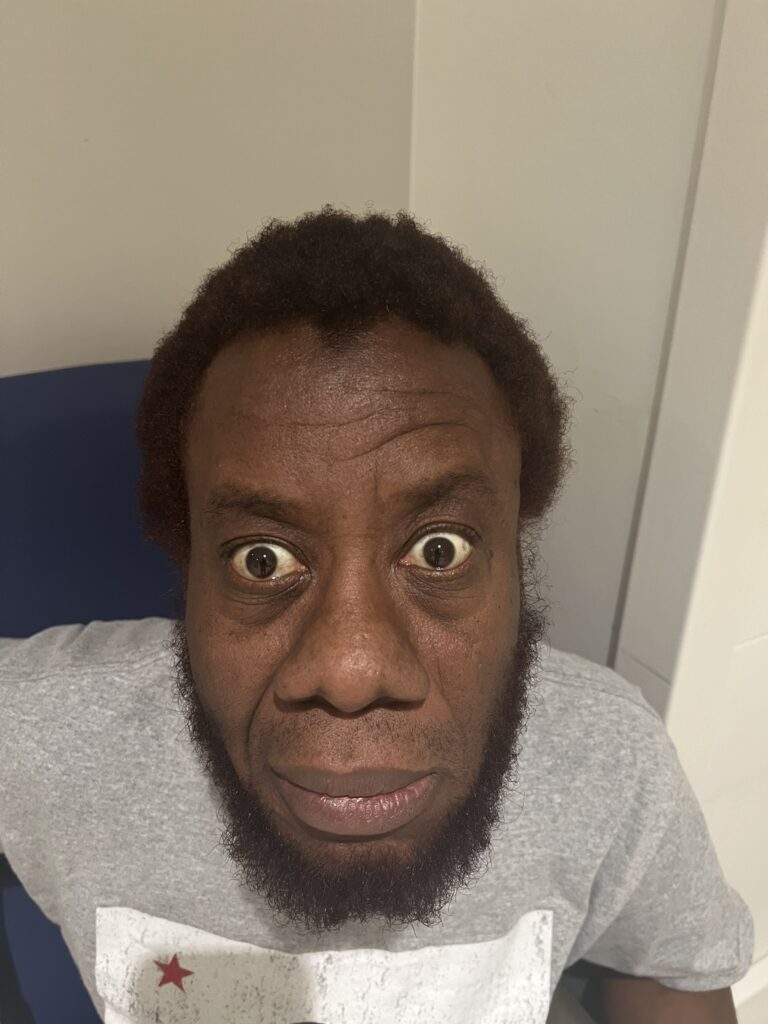
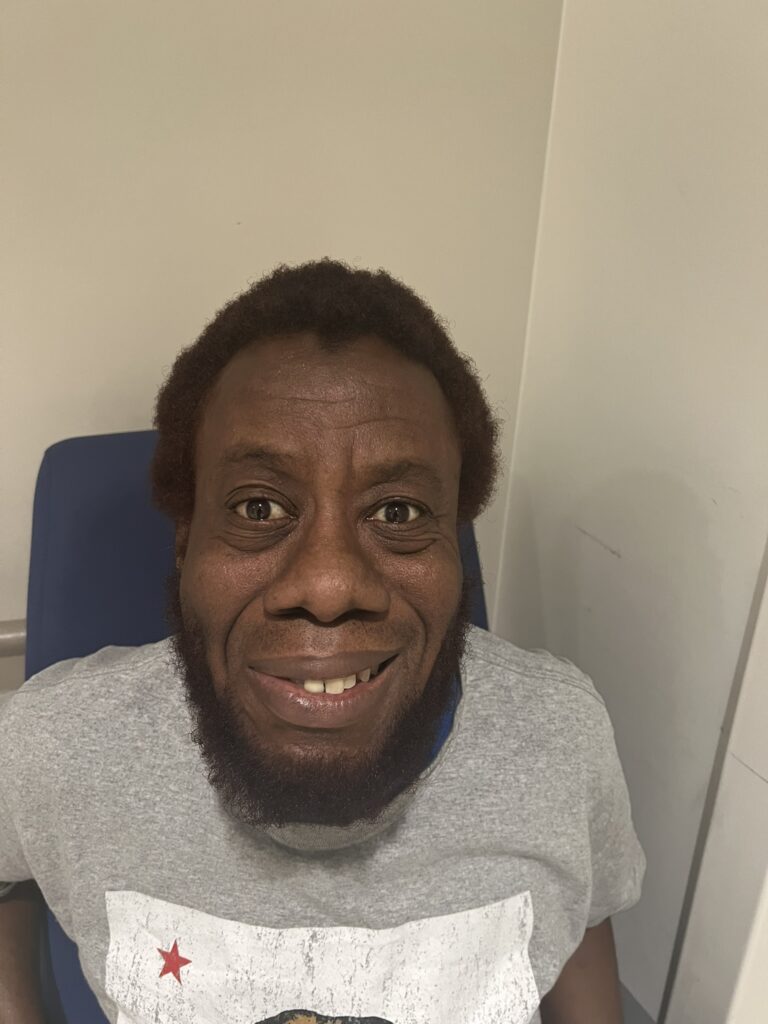
- Face
- General
- Plethoric (secondary polycythaemia)
- Telangiectasia (systemic sclerosis)
- Butterfly rash (SLE)
- Lupus pernio (Sarcoidosis)
- Eyes
- Conjunctival pallor
- Horner’s syndrome (miosis, ptosis – Pancoast tumour)
- Episcleritis (RA)
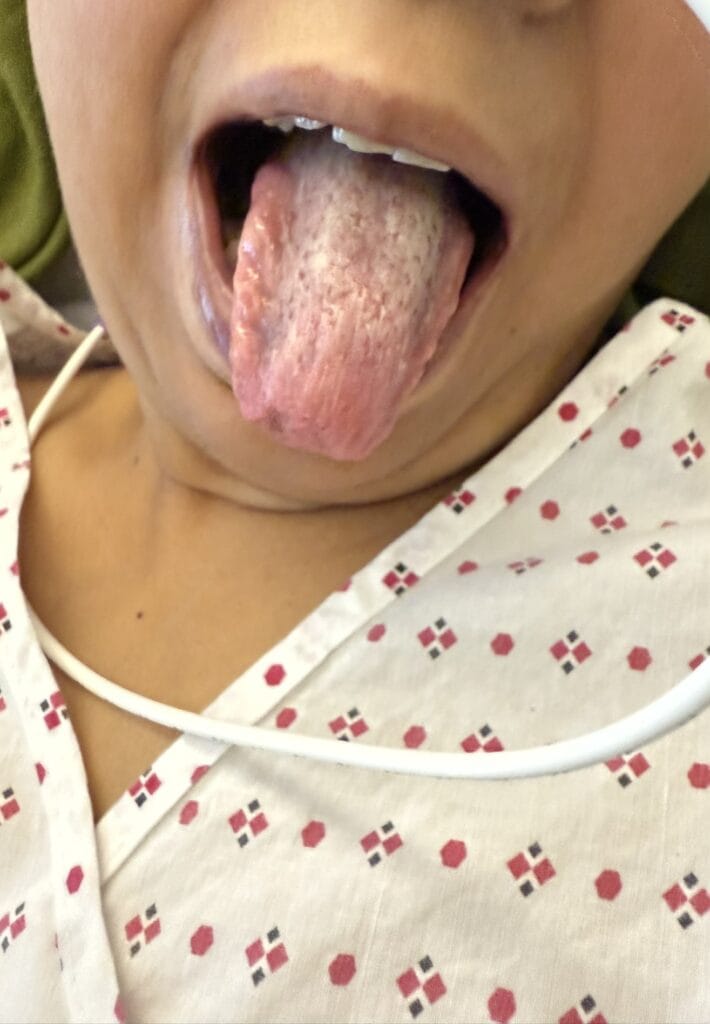
- Mouth
- Central cyanosis under tongue (hypoxia)
- Telangiectasia (systemic sclerosis)
- Microstomia (systemic sclerosis)
- Neck
- JVP (raised in cor pulmonale)
- Tracheal deviation
- Cricosternal distance (< 3 fingers in COPD)
- Cervical lymphadenopathy
- General
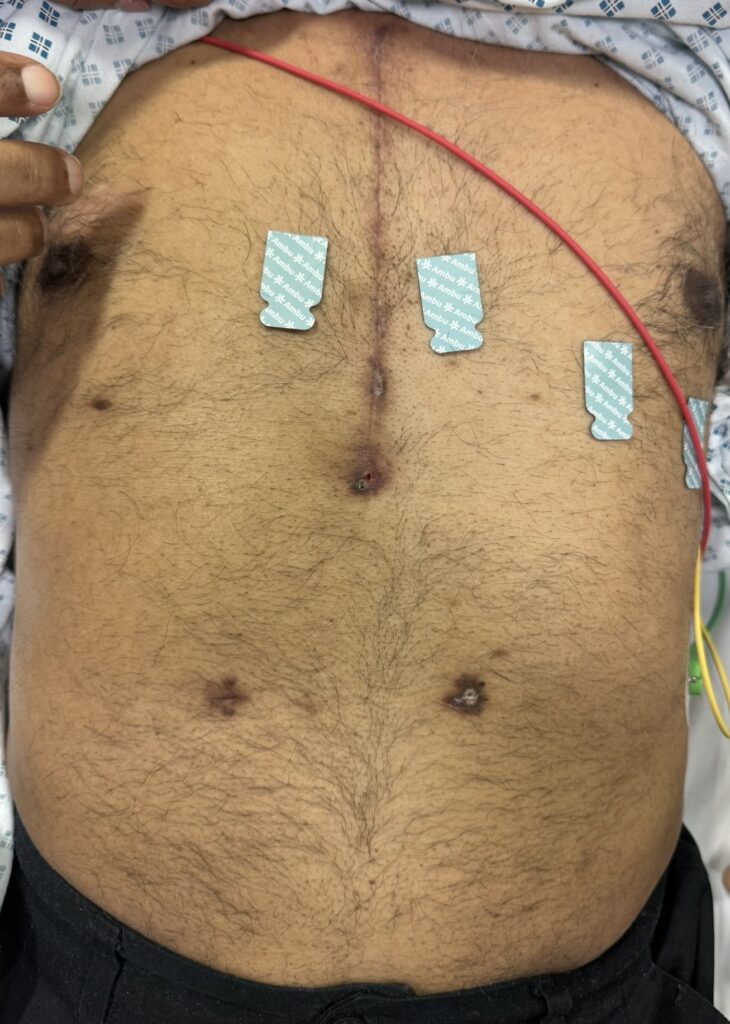
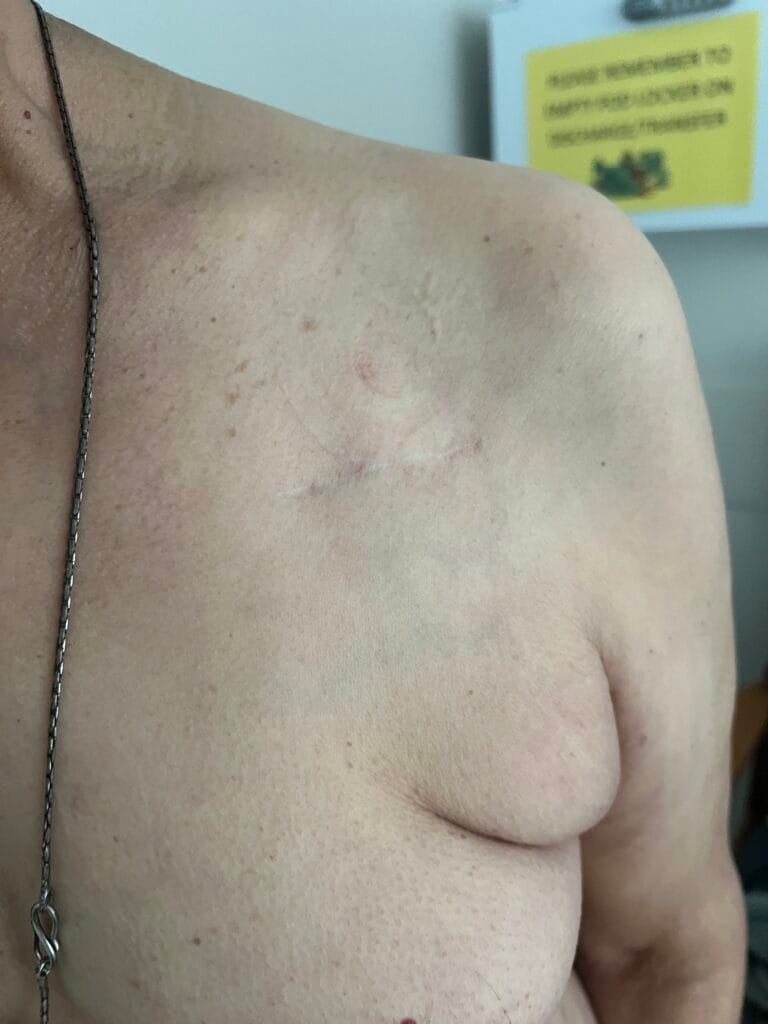
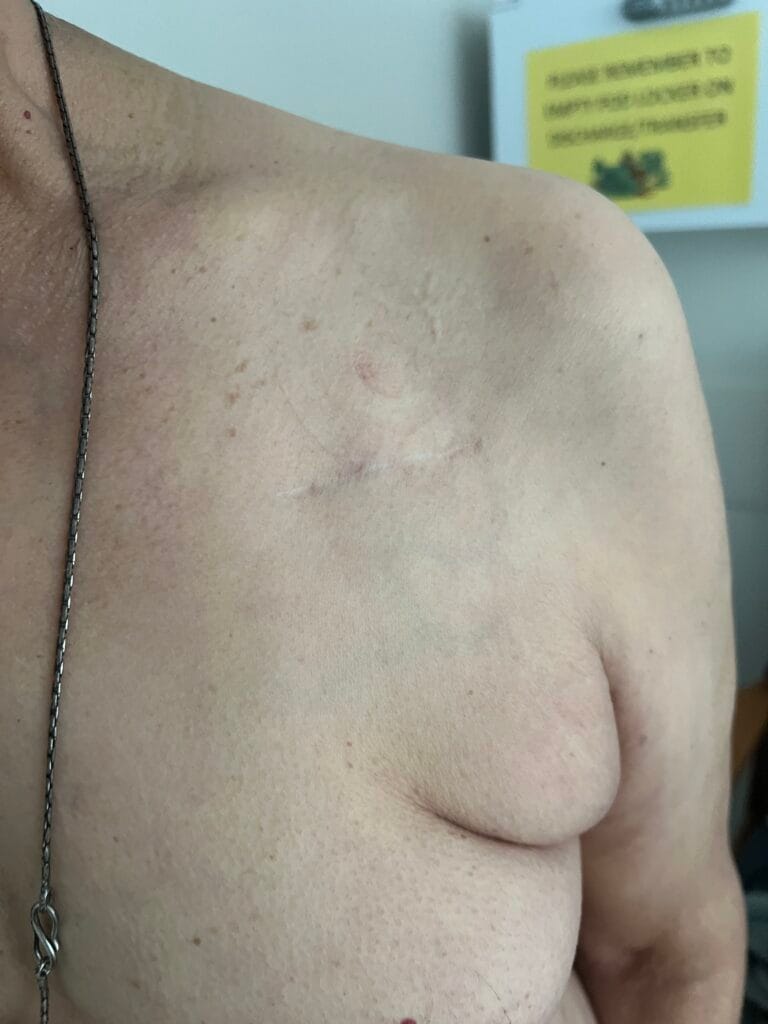
- Torso
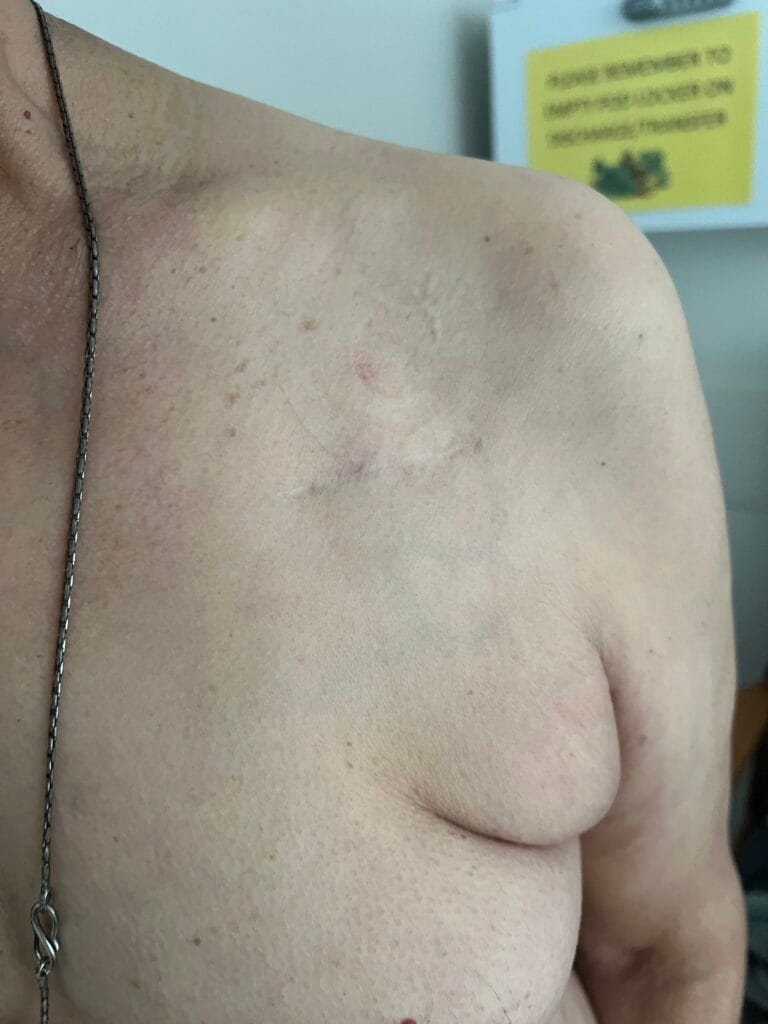
- Posterior thoracotomy scar (lung transplant, lobectomy)
- Chest drain scars (look close safety triangle)
- VATS scars
- Asymmetrical chest expansion (fibrosis)
Peripheral oedema (cor pulmonale)
Chest:
- Bilateral bi-basal fine end-inspiratory crackles🔊 fixed non-altered by coughing
- Reduced chest expansion
Presentation:
Diagnosis: Clinical findings are consistent with a diagnosis of interstitial lung disease affecting the upper/
lower zones as evidenced by:
Most pertinent positive findings are: [Important Physical Signs]
- Audible bilateral end-inspiratory crackles in upper/lower zones fixed with coughing
- Finger Clubbing
- Rheumatoid hands and extensor nodules
Reduced chest expansion
The most likely underlying cause of ILD in this patient is:
- Rheumatoid Arthritis (peripheral symmetric deforming polyarthropathy)
- Systemic Sclerosis (telangiectasia,Sclerodactyly, Microstomia)
- SLE (butterfly rash, arthropathy)
Idiopathic pulmonary fibrosis (Clubbing)
Important negative findings include:
- No evidence of acute respiratory failure with absence of peripheral or central cyanosis.
- No signs of pulmonary hypertension (loud P2, RV heave, TR)
- No evidence of cor pulmonale with no overt JVP rise, no RV heave and no peripheral oedema.
No evidence of CO2 retention with absence of CO2 flap.
To complete my examination I would like to measure oxygen saturations at rest, perform a peak flow test and
obtain full drug and social/occupational history.
Differential Diagnosis:
There is a wide differential diagnosis here but what may be relevant to this particular patient is:
- Pulmonary oedema secondary to left ventricular failure
- Bronchiectasis (coarse crackles that change with coughing +/- wheeze)
- Suppurative lung disease (consolidation, abscess)
Lung malignancy
Classification of interstitial lung disease
- Exposure
- Drugs (Methotrexate, Amiodarone, Bleomycin, Nitrofurantoin, Phenytoin, Cyclophosphamide)
- Occupational (Asbestosis, Coal pneumoconiosis, Silicosis)
- Hypersensitivity Pneumonitis
- Connective Tissue Disease
- Rheumatoid Arthritis
- Systemic Sclerosis
- SLE
- Polymyositis/Dermatomyositis
- Sjogren’s
- Vasculitis (eosinophilic granulomatosis)
- Sarcoidosis (upper zone)
- Ankylosing Spondylitis (upper zone)
- Idiopathic
- Idiopathic pulmonary fibrosis
- Acute interstitial pneumonia (AIP)
- Non-specific interstitial pneumonia (NSIP)
- Post-infection (asymmetrical fibrosis) [upper zone]
- TB
- ABPA
- Fungal
Clinical Judgement:
Bedside tests:
- ABG – checking for type 2 respiratory failure
- ECG – looking for right heart strain
- Oxygen saturations
Serial peak flow measurements
Blood investigations:
- FBC (polycythaemia in chronic hypoxia)
- Inflammatory markers (CRP and ESR)
- Autoimmune screen (ANA, anti-ds DNA, anti-Scl, RF, anti-CCP, ANCA)
- Serum precipitins (hypersensitivity pneumonitis)
- Serum ACE and adjusted calcium levels (Sarcoidosis)
- Aspergillin RAST test, IgE specific to Aspergillus
- Urea and electrolytes (drug-related ILD nephrotoxicity)
Liver function tests (liver derangement with antifibrotics)
Imaging Studies:
- CXR – bilateral reticulonodular interstitial infiltrates
High Resolution CT Chest – ground-glass opacifications (NSIP), honeycombing (UIP)
Special tests:
- Pulmonary Function Tests
- Spirometry (FVC, FEV1, FEV1/FVC ratio – restrictive defect)
- Lung volume plethysmography (reduced volumes FVC < 80% to assess suitability for
antifibrotics, FEV < 1 unsuitable) - 6-minute Walk Test (desaturation)
- Diffusion Capacity of Lungs for CO
- Transfer factor and lung coefficient factor reduced
- High DLCO : asthma, obesity, pulmonary haemorrhage, polycythaemia, leftright shunt
- Low DLCO : Lung resection, ILD, emphysema, anaemia, pulmonary
vascular disease
- Transfer factor and lung coefficient factor reduced
- Bronchoalveolar Lavage for cell types and cytology (lymphocytosis responsive to steroids in NSIP,
eosinophilic pneumonia, asbestos bodies, malignant cells) - Video-assisted transbronchial biopsy
- Echocardiogram to assess for pulmonary hypertension (RV hypertrophy, elevated RV systolic
pressure) - Right Heart Catheterisation (mean Pulmonary Artery Pressure > 25mmHg in PAH)
Management
- MDT approach following referral to specialist tertiary centre
- Treat underlying cause
- Conservative
- Patient Education
- Lifestyle interventions – alcohol cessation, smoking cessation, encourage physical activity,
balanced diet, vaccinations (pneumococcus, influenza, COVID-19) - Remove causative allergen/agent
- Pulmonary rehabilitation
- Medical
- Anti-fibrotic (pirfenidone) [FVC 50-80%, drop in FVC > 10% in 6/12]
- Tyrosine kinase inhibitors (nintedanib)
- Steroids and immunosuppression in CTD
- Long-term Oxygen Therapy
- Surgical
- Single or double lung transplant
- Manage complications
- Infective exacerbations
- Pulmonary hypertension (Group 3 – secondary to lung disease and hypoxia)
- Respiratory failure (Type 2 Respiratory Failure – restrictive defect)
Lung cancer
Indications for lung transplant:
Single:
- Emphysema
Idiopathic pulmonary fibrosis
Double:
- Cystic fibrosis
- Bronchiectasis
- COPD (A1AT deficiency)
Pulmonary hypertension
Heart-Lung Transplant
- Eisenmenger syndrome (transposition of great arteries, truncus arteriosus, atrioventricular canal)
Primary pulmonary hypertension (PAWP > 25mmHg)
Absolute contraindications:
- Disseminated malignancy
- Critical illness (major organ dysfunction)
- Ventilator dependent
- Current smoker
Poor social support network
Extra-articular manifestations of Rheumatoid Arthritis
- Cardiovascular
- Pericarditis
- Vasculitis
- Pulmonary arterial hypertension
- Pulmonary
- Interstitial lung disease
- Bronchiolitis obliterans
- Pleural effusions
- Caplan syndrome (pulmonary nodules and pneumoconiosis with dust inhalation)
- Pleuritis
- Neurological
- Cervical myelopathy (C1-C2 subluxation seen on flexion-extension cervical radiography)
- Peripheral neuropathy
- Mononeuritis Multiplex (foot drop)
- Carpal tunnel
- Metabolic
- Osteoporosis
- Steroid induced diabetes mellitus
- Haematological
- Anaemia (chronic disease, methotrexate myelosuppression, NSAID gastropathy, Felty’s)
- Felty’s syndrome (RA, splenomegaly, neutropenia)
- Amyloidosis
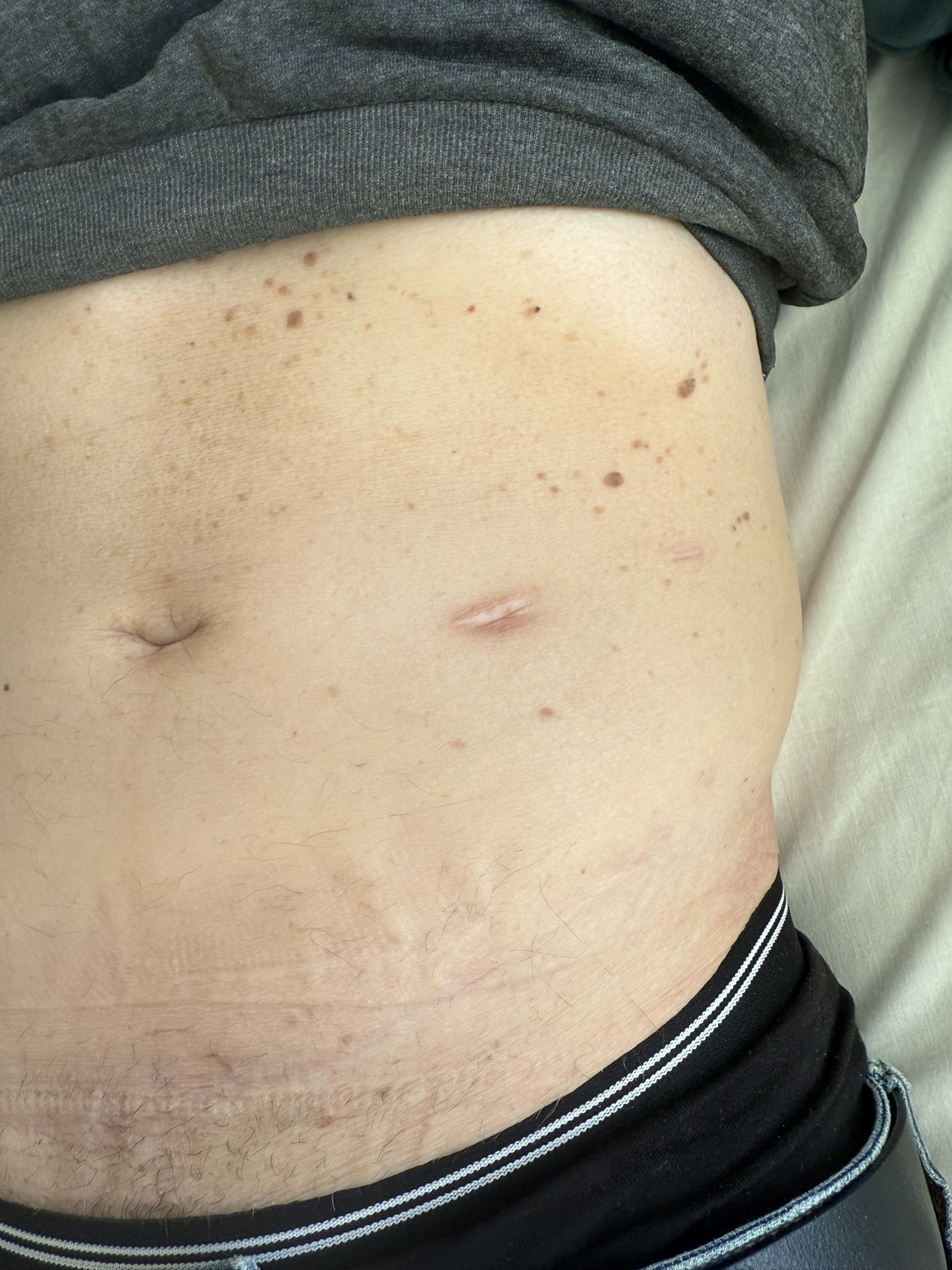
- Skin
- Rheumatoid nodules (firm or rubbery nodules on pressure areas i.e. olecranon)
- Eyes
- Episcleritis/scleritis (acute red painful eye)
- Keratoconjunctivitis sicca (secondary Sjorgren syndrome)